Migraines can be particularly challenging for women undergoing hormonal transitions like perimenopause and menopause. Understanding the interplay between these hormonal changes and migraine management is crucial for effective treatment. This blog explores the use of hormone replacement therapy (HRT) and triptans, comparing their efficacy and providing insights into lifestyle changes that can help alleviate symptoms.
Hormone Fluctuations and Migraines in Perimenopause and Menopause
Hormone Fluctuations and Migraine Prevalence
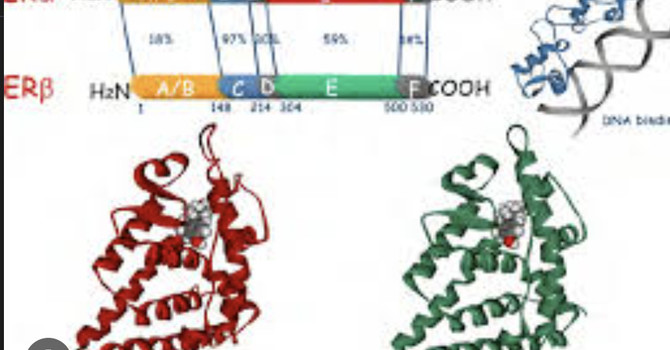
Migraine prevalence and severity are significantly influenced by hormonal fluctuations, particularly estrogen levels. During perimenopause, the transition phase leading up to menopause, women often experience irregular menstrual cycles and erratic fluctuating hormone levels, which can exacerbate migraines. This period is marked by increased frequency and severity of migraine attacks, especially in women with a history of menstrual migraines. The unpredictable nature of estrogen levels during perimenopause is a key factor in the worsening of migraines during this time .
Few studies specifically address the epidemiology or treatment of migraines in midlife women. However, clinical observations and epidemiologic studies suggest that migraines generally worsen during the menopause transition and improve post-menopause. Perimenopause-related increases in comorbid conditions (anxiety, depression, sleep disturbances) also may contribute to worsening of migraines. The association between perimenopause and migraine exacerbations appears most pronounced in women with a history of menstrual migraine and declines after menopause, with stabilization and lowering of endogenous estrogen levels . In contrast with spontaneous menopause, induced menopause, including surgical menopause, appears to be associated with an increase in the frequency or intensity of migraines .
Menopause and Migraine
As women transition into menopause, characterized by the cessation of menstrual periods and a more stable, low level of estrogen, many report an improvement in migraine symptoms. However, the transition itself can be challenging due to hormonal instability . Postmenopausal women generally experience fewer migraines, although this improvement is more pronounced in those who undergo natural menopause compared to surgical menopause. Some women will continue to experience migranes well into menopasue.
Hormone Replacement Therapy (HRT) and Migraine Treatment
Benefits of HRT
Hormone Replacement Therapy (HRT) can be beneficial in managing migraines during perimenopause and menopause by stabilizing estrogen levels. Continuous administration of low-dose estrogen, particularly via non-oral routes like transdermal patches, creams or oils , can help mitigate the frequency and severity of migraines associated with estrogen withdrawal . HRT is also effective in alleviating vasomotor symptoms such as hot flashes and night sweats, which are common during menopause .
Risks and Considerations
In some women high doses of estrogen can exacerbate migraines, particularly those with aura. It is imperative to indiviualize care and recognize that each woman will heave her own hormnal needs. . Additionally, continuous rather than cyclic administration of progestogens is preferred to avoid triggering migraines .
Alternative Treatments
For women who cannot or choose not to use HRT, non-hormonal treatments such as serotonin reuptake inhibitors (e.g., venlafaxine, fluoxetine) and gabapentin have shown efficacy in managing both vasomotor symptoms and migraines . Lifestyle modifications and non-prescription treatments like isoflavones may also provide some relief, although evidence is limited .
Triptans for Migraine Management
Efficacy and Mechanism
Triptans are considered the first-line treatment for acute migraine attacks. They work by targeting serotonin receptors to constrict blood vessels and reduce inflammation, providing pain relief within 2 hours for 42-76% of patients .
Research Findings
- Acute Treatment: Triptans are highly effective for treating menstrual migraines and are available in various formulations (oral, nasal, injectable) .
- Preventive Use: Some studies have explored the use of triptans for short-term prevention of menstrual migraines when taken perimenstrually .
- Safety Considerations: Triptans are generally safe but have contraindications for patients with certain cardiovascular conditions .
Comparing HRT and Triptans
Treatment Approach
- HRT: Primarily used for overall hormone stabilization and may have a preventive effect on migraines. It is also used to manage other menopausal symptoms like hot flashes and night sweats.
- Triptans: Used for acute treatment of migraine attacks, including menstrual migraines. They provide fast-acting relief and can be used for short-term prevention around menstruation.
Long-term vs. Short-term Use
- HRT: Considered for longer-term management of menopausal symptoms, including potential migraine prevention.
- Triptans: Used for shorter durations, primarily for acute relief or short-term prevention.
Lifestyle Changes to Alleviate Symptoms
In addition to medical treatments, several lifestyle modifications can help manage both migraines and menopausal symptoms:
- Diet: A balanced diet rich in fruits, vegetables, whole grains, and healthy fats can support overall health and reduce migraine triggers. Avoiding known triggers like caffeine, alcohol, and processed foods is also beneficial.
- Exercise: Regular physical activity, including aerobic exercises, yoga, and Tai Chi, can reduce stress and improve overall well-being, which may help in managing migraines and menopausal symptoms.
- Sleep: Maintaining a consistent sleep schedule and ensuring high-quality sleep are vital for migraine management. Poor sleep can exacerbate both migraines and menopausal symptoms.
- Hydration: Staying well-hydrated is essential, as dehydration is a common migraine trigger.
- Stress Management: Practices such as meditation, deep breathing exercises, and progressive muscle relaxation can help manage stress, a known trigger for migraines.
Conclusion
Managing migraines during perimenopause and menopause involves a combination of medical treatments and lifestyle changes. HRT can be effective for some women by stabilizing hormonal fluctuations, it may worsen migraines in others thus individualized care is important. Triptans remain the gold standard for acute treatment of migraine attacks, including menstrual migraines, and can also be used for short-term prevention.
The choice between HRT and triptans depends on various factors, including the patient's overall health, migraine pattern, and other menopausal symptoms. Some women may benefit from a combination approach, using HRT for overall hormone stabilization and triptans for acute attacks. Consultation with healthcare providers specializing in both headache management and menopause is crucial for optimal care.
By understanding the interplay between hormonal changes and migraine management, women can make informed decisions about their treatment options and improve their quality of life during perimenopause and menopause.
Dr. Anat Sapan MD, specializing in peri/menopause care, advocates for a personalized approach combining Bioidentical Hormone Replacement Therapy with lifestyle strategies. Her telemedicine services in California, Florida, Illinois and New York. I aim to help women overcome menopausal symptoms and enhance their quality of life.

Anat Sapan, MD
Contact Me